Reflections of a Mayo Medical Student Volunteer at Bwindi Community Hospital

Most people dream of visiting sandy beaches or luxury resorts for their honeymoon. When I brought up the idea of traveling to rural Africa for a medical volunteer trip, my soon-to-be husband was not exactly keen. He has a distinct fear of bugs and prefers fine dining to the outdoors. Yet six months later and newlywed, we found ourselves boarding a flight to Uganda.
My name is Liz, and I came to Bwindi Community Hospital (BCH) as a volunteer physician from Mayo Clinic. Engaging in global health has been a dream of mine for many years, and I finally felt prepared after completing internal medicine residency and beginning a new chapter of fellowship in preventive medicine and public health. I would be sharing this adventure with my new husband, Tyler. He is in his final year of ophthalmology residency at Mayo Clinic, and he will try almost anything to make me happy (including a honeymoon in Uganda).
Our travel itinerary was the longest either of us had ever experienced: a flight from Miami to Chicago, Chicago to Brussels, then Brussels to Kigali, Rwanda. After spending the night in Kigali, we had a 6-hour car ride the next morning through winding dirt roads to reach Bwindi. We had feared the long ride, but it was just the start of our adventure as locals welcomed us waving from the road and children chased after the vehicle carrying “mzungu” (the local word for light-skinned visitors).
We reached the BCH guest house near dinner time and had our first Ugandan meal: goat meat with vegetables and rice. The guest house is a haven for hospital volunteers and travelers, and conversation flows in various accents across the long community tables. Dinner regularly gives way to card games or occasionally movie night. Evenings at the guest house also offer time to catch up on work or to make plans for weekend safaris or gorilla trekking. One thing is clear: at the guest house, you are family.
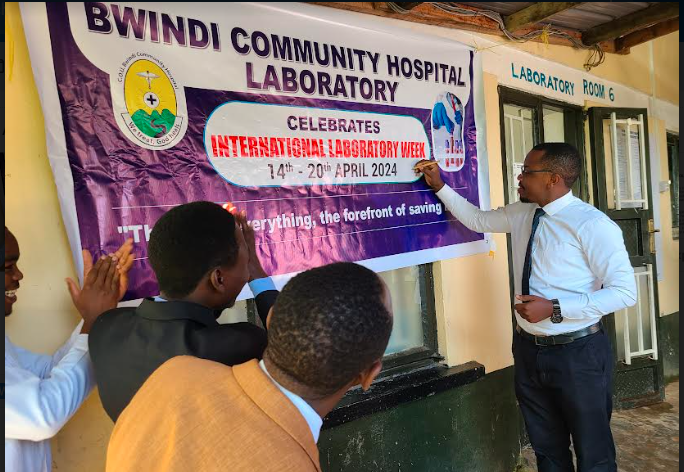
Monday morning came quick. The workday at BCH starts with rounds, but not in the traditional sense. At 8am, rounds kickoff with drumming, clapping, and singing. Prayers follow, and then medical announcements for the hospital are made. This particular week was a celebration of “BCH Lab Week,” and we were graced with a special performance of the Ugandan national laboratory workers’ anthem. I highly recommend listening on YouTube.
After rounds, the bustle begins. Patients have traveled from near and far to visit BCH, and they often plan to be there for the full day. They arrive with bundled babies on their backs or relatives in tow. As the patient queue grows, medical staff and volunteers disperse to various parts of the hospital by specialty. Throughout the week, I spent time in the inpatient medical ward, outpatient department, chronic care clinic, HIV/TB clinic, and with community outreach. Tyler remained committed to his post in the eye clinic.
Both of us were struck by the culture shock of practicing medicine without our usual tools. Dr. Alex told me on the first day of medical wards, “You must use your imagination to envision what is going on inside the patient.” This proved difficult as an American doctor who relies heavily on daily bloodwork, CT scans, and pathology reports. I grew to appreciate the importance of my history and physical exam to detect clinical clues, and I learned to recognize signs of endemic diseases, such as tuberculosis and malaria. Implementing screening and prevention for HIV and TB became part of my daily practice as the Ugandan Ministry of Health tracks the spread of these infectious diseases closely.
I felt at home managing patients with hypertension and diabetes in chronic clinic. I learned that these chronic diseases are becoming more prevalent in Uganda, but there are not yet screening guidelines that compare to those in the U.S. By some estimates, up to 89% of Ugandans with diabetes are unaware of their diagnosis. I can’t help but wonder if prevention and screening guidelines will evolve to address this issue as chronic diseases replace infectious diseases as the major cause of morbidity and mortality in Uganda.
In eye clinic, Tyler honed his exam skills. He saw unique presentations of uveitis, glaucoma, cataracts, and macular degeneration. One particularly challenging case saw him surgically repairing a complex eyelid laceration. In addition to clinical skills, Tyler used his mechanical skills to restore a broken autorefractor machine for the eye clinic. This machine allows users to easily generate vision prescriptions, which will impact many patients to come.
Our time at BCH is ending, and we feel sad to be leaving a place that has challenged us but also made us feel so at home. Every day here we are greeted with smiles, handshakes, high-fives, “bongas” (fist bumps), and hugs from patients and staff alike. As the hospital embarks on building its new vision clinic, Tyler hopes he can help advise what tools would be beneficial for the community. Similarly, I would like to influence the development of chronic disease prevention initiatives at BCH. Knowing there is still work to be done, we are hopeful to keep in touch with our new friends here and to return someday soon.
Aurthor: Liz Lees